9. Survivorship and Rehabilitation
You have a right to:
Receive and discuss with your care team a clear, managed and achievable plan for your survivorship and rehabilitation.
Three key questions that every cancer patient may choose to ask:
- Will our cancer service help me face my challenges as a cancer survivor?
- Will I be given a survivorship care plan to help me cope with any problems I may encounter as a cancer survivor?
- How do I access supportive and rehabilitation help for cancer survivors?
Explanation
European cancer patients’ care should be supported in their needs as a cancer survivor. In response to the growing number of people surviving cancer in Europe, there has been increasing focus on the quality of survival. In this setting, “survivorship” has various definitions. It can include anyone diagnosed with cancer and include their entire cancer journey. More often, the focus will be on patients’ survival from the period of time after they complete their active treatment. However, preparations to support survivorship can begin before active treatment is completed. A number of patient advocacy organisations have extensive experience in this area and patients should be referred to these organisations for information on support groups and guidelines, including on work- and finance-related issues.
Cancer and its treatment can have a considerable and long-term impact on everyday life. Some cancer survivors may face a range of challenges including physical problems, poorer quality-of-life, psychological distress, sexual problems, problems with social relationships and financial concerns. Some consequences may emerge five or ten years after treatment (late effects) and can have a significant impact. For example, cancer patients may be at greater risk of a second cancer; some chemotherapy can increase the risk of heart disease, and long-term hormone therapy can sometimes be related to development of osteoporosis.
Supporting cancer survivors includes providing psychosocial aspects of support, such as coping with disruption to one’s life, managing the consequences of treatment, living with uncertainty and lifestyle changes. Being a cancer survivor may disrupt one’s social and sexual roles and identity. Patient advocacy organisations can offer significant help to support the cancer survivor.
High-quality cancer care should include an active approach to the challenges that patients face as cancer survivors. Every patient should be given a survivorship cancer plan, prepared for them in consultation with their cancer care professionals and fully explained. Patient advocacy organisations have a lot of experience in the practical issues that arise (eg relating to work, travel, leisure activities etc) and should be consulted. It is important that the cancer professionals and patients together identify and discuss any particular risks that the individual may have; specific approaches can then be taken to reduce those risks. These may include lifestyle changes such as giving up smoking, maintaining exercise, ensuring good nutrition and a healthy body weight. They may also involve medical follow-up measures including screening for the late complications of cancer and its treatment. Supportive care should be available for those patients who experience psychological distress, sexual or social problems as well as for those who have physical problems or late complications of the treatment or the disease. Survivorship care plans should be regularly reviewed and updated to reflect changes in circumstances and evolving life goals.
Supporting Literature and Evidence
The substantially increasing number of cancer survivors in Europe led the EU Joint Action on Cancer Control (CanCon) to focus on survivorship and rehabilitation as part of the European guide on quality improvement in comprehensive cancer control (5, 187). The European Organisation for Research and Treatment of Cancer (EORTC) has highlighted the importance of survivorship and addressing this need through research and innovation (53, 188-191). The European Cancer Organisation has established a Survivorship and Focussed Topic Network (13). The objective of these and a wide range of other survivorship initiatives worldwide was to take into account the psychosocial needs of patients and improve QoL for cancer patients through support, rehabilitation and palliative care improving coordination and communication.
In describing cancer survivorship, CanCon drew on the definition provided by the US National Coalition for Cancer Survivorship (192) which describes it as ‘the experience of living with, through and beyond a diagnosis of cancer’. This inclusive definition means that a cancer survivor is anyone who has had a diagnosis of cancer and who is still alive. The definition of a survivorship plan by the US National Cancer Institute was ‘A detailed plan for a patient’s follow-up care after treatment for a disease ends (193).” In preparing the European Code of Cancer Practice, we have focused on the period of time after some active cancer treatment has been successfully finished. All divisions are quite artificial and an awareness of survivorship-related issues should be maintained at all parts of a patient’s journey.
In Europe during the last 6 years, there have been tremendous increase of awareness of new survivorship challenges faced by cancer patients leading to the involvement of policy makers in order to adapt the legal framework related to the financial challenges that they face. Innovative measures have been taken in France in 2016, in Belgium in 2018, and in Luxembourg as well as the Netherlands in 2020 establishing a “right to be forgotten” such that they do not face discrimination as a consequence of their cancer diagnosis and treatment. (15, 16, 194-195). However, there is a need to provide equal access to all Europe’s cancer survivors to such legislation and to put an end to discrimination throughout Europe. Recently, major steps forward have been taken by the EU Commission (15-16) to clearly stress the need for a “right to be forgotten” which is encouraging for all cancer patients.
The CanCon Report identified the importance of the advice from the Institute of Medicine that specific templates for a survivorship care plan should be developed for the follow-up of cancer survivors and used in the development of survivorship care plans to overcome the many factors impeding good QoL for cancer survivors (187, 196-197). It is clear, however, that such care plans are still used to only a modest degree, because of the difficulty of integrating them into practice and the resources required to do so. The best approaches employ survivorship care plans that cover both medical and non-medical aspects of care. Models reported include the shared care model and the availability of specialized survivorship clinics. Evidence suggests that there is considerable added-value for patients and healthcare systems with the use of survivorship care plans even though they are currently far from routinely employed (198).
CanCon identified six key areas for survivorship planning:
- Medical follow-up: management of late effects, and tertiary prevention
- Palliative care in primary and secondary care
- Psychological support
- Social rehabilitation including employment issues
- Empowerment of cancer survivor
- Multidisciplinary approach and coordination of care providers
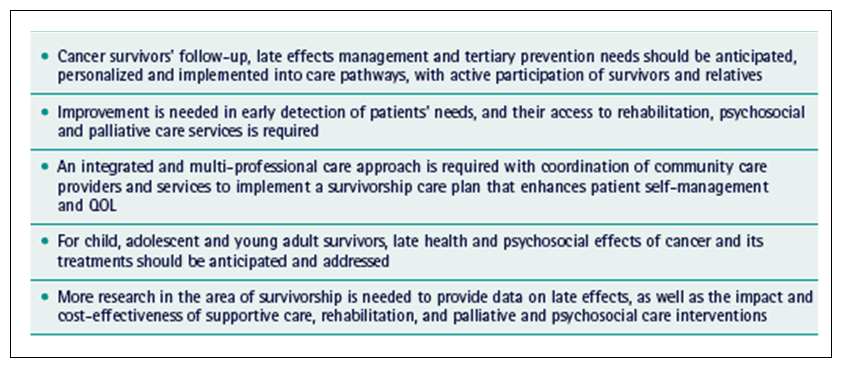
The main messages from the CanCon project are shown in Table 11.
Table 11. The main messages from the CanCon Member State Joint Action Against Cancer (5)
Survivorship care plans have to take account of the need to assess the direct and indirect effects of cancer and its treatment, such as specific organ toxicity, fatigue, pain, depression, anxiety, sleep disturbances, and sexual or fertility problems. Patients need to be directly asked about these important aspects of their survivorship by systematic collection via PROM measures. Social issues [The Code 7] may be very pressing for cancer patients. CanCon emphasised a multidisciplinary, patient-centred approach to survivorship care. Key aspects include clarity around an early and personalized follow-up programme agreed with each cancer survivor; the use of adequate and updated information on long-term effects provided to cancer survivors; the integration of tertiary prevention into the plan and a patient-centred approach to the provision of care, including psychological and social support and a focus on maintaining QoL.
Self-management support can help patients to manage the issues they face as cancer survivors, as active partners, working in collaboration with healthcare providers. They should be supported to build knowledge, skills, confidence and resilience to manage the impact of symptoms and limitations in order to live a full and meaningful life. They should be enabled to access support within and beyond health services to better manage health and well-being. People need varying degrees of support from healthcare professionals and others to achieve this (187, 198).
Fertility issues
Approximately 10% of newly diagnosed cancers occur in individuals aged between 15 and 49 years, which together with the trend towards delayed childbirth means more people are diagnosed with cancer before their families are complete, and an increased proportion of survivors are concerned about fertility issues (199). The effects of surgery, chemotherapy and radiotherapy on fertility have been well documented and other treatments can have direct or indirect effects. Increased concerns about fertility have been correlated with increased psychological morbidity. Among breast cancer survivors, 57% recalled substantial concern at diagnosis about infertility (200). In women with ovarian cancer, approximately 50% feared reduced ability to reproduce (201). Among young men newly diagnosed with cancer, having children ranked as their third highest priority (202). Many barriers have been identified in discussing fertility issues with cancer patients. They include physicians prioritizing treatment issues rather than QoL after treatment, lack of knowledge of fertility preservation and concerns over delays in treatment (199). Consideration of referral to a fertility specialist should be incorporated into the multidisciplinary team (MDT) strategy, with clear protocols to incorporate appropriate fertility treatment.
Psychosexual issues
Prevalence rates of sexual difficulties associated with cancer and its treatment vary widely, depending on the primary diagnosis, treatment modality, method(s) of assessment and threshold criteria for severity and type of sexual dysfunction. For example, over 50% of people with pelvic cancer experience disruption to their sexual well-being. Anxiety and depression, body image adjustment, altered femininity or masculinity, infertility concerns, relationship strain and broader social difficulties are also precipitating and maintaining factors for sexual difficulties. Discussing the sexual consequences of cancer is difficult for health professionals and patients alike. The increased use of brief approaches to screen patients for psychosexual problems and the use of PROMs may assist busy clinicians to introduce and structure clinical discussions. Sexual difficulties may improve over time and the best management often involves biomedical, psychological and relationship strategies (203).