3. Quality of Care, Expertise and Best Outcomes
You have a right to:
Information about the quality and safety of care, the level of expertise and the outcomes achieved for your type of cancer in the centre where you are being treated.
Three key questions that every cancer patient may choose to ask:
- Will my diagnosis and treatment be managed by a team of healthcare professionals with the necessary expertise to give the best advice and identify the best available options for me?
- Is that team specialised in the particular cancer with which I have been diagnosed?
- Does my healthcare team keep records of their clinical outcomes which I may see in an anonymised format, and will I be able to compare those outcomes to those achieved by similar teams in similar institutions?
Explanation
European cancer patients should be given access to information about the care provided and the outcomes achieved by their specific cancer healthcare team. This is essential to allow patients to take informed decisions about their treatment and where it is delivered.
Different healthcare professionals deliver specific aspects of a patient’s diagnosis and care. While primary care and general practice healthcare professionals have skills that can help in identifying suspicious symptoms, referring patients for a cancer diagnosis and supporting the individual through their healthcare journey, they will not have specialised cancer treatment expertise. Specialised cancer care should be given by a team of healthcare professionals with expertise in a specific cancer and its treatment in a hospital or a dedicated cancer centre. Patients have the right to know the level of expertise and experience of healthcare professionals and teams who will be looking after them. Therefore, they need access to information about the results their healthcare team have achieved, for their specific cancer, and how it compares to expected results from other hospitals or cancer centres.
In order to achieve the best results for patients, their specialist care team must have substantial experience across a broad range of professional competencies. They must be well led and coordinated, have adequate resourcing and participate in training programmes to maintain and upgrade their skills. Professional organisations across Europe recommend the required level of activity and competency which is appropriate for a team (eg number of patients with that particular cancer type cared for by the team per year), to ensure the best results for patients. Application of the available European Cancer Organisation’s Essential Requirements for Quality Cancer Care can help support the delivery of best available care.
Care teams should regularly audit their results and compare them to other similar teams in other institutions. However, comparisons between teams and their outcome results is not always straightforward, as different teams may be dealing with patients at different stages of their cancer and be using different treatments. Nonetheless, informative, careful comparisons are possible and this process ensures that the care team is continuously looking to improve and achieve the best outcomes for patients across all indicators of the quality of the care provided. This information should be made publicly available and accessible to patients to consider when they are making their decisions on treatment options and should be published by healthcare institutions, government departments and/or professional organisations.
Supporting Literature and Evidence
Central to the definition and evaluation of good clinical cancer practice is the availability of high-quality clinical data indicating the outcomes for patients undergoing care at cancer centres and hospitals at a national, regional and local level. Only through having access to such high-quality data is it possible to sustain and develop models of good clinical cancer practice that are appropriate for each country and ensure that each patient is receiving the best available care.
Patients need access to the data in order to judge whether the service providing their own care is working effectively to give the best possible outcomes; healthcare professionals need the data to audit their results and determine how they can improve their practice; healthcare managers need the data to evaluate the effectiveness and value of the service they provide; policymakers need good data to underpin their present and future policy initiatives. The collection of good quality data, eg by providing easy-to use and interoperable IT systems (and support by data managers) is a prerequisite to obtain the data needed to underpin the provision of good cancer care. This is not always the case at the moment, in hospitals or healthcare systems.
The provision of information to support cancer patients in their choice of centres and to provide detailed information on the activity and outcomes in different cancer centres and hospitals is principally conducted at a national level. A patient’s individual service should be able to provide a point of access to this information. An example of a national information source on the volume of surgery for cancer surgery is Italian Oncoguida (115). The Italian Oncoguida is an information service produced by the Italian Association of Cancer Patients (AIMaC) in collaboration with the Italian Institute of Health and the Italian Ministry of Health. Oncoguida provides detailed, patient-oriented information on Italian hospitals and cancer centres providing cancer care, including volume of surgeries performed per tumour site, availability of psychological and physical rehabilitation services and contact details of patient associations involved at the hospital level.” (5). The Italian Association for Cancer Patients, Relatives and Friends (AIMaC) provides a wide ranging source of support (116). They provide a national helpline, 40 cancer information desks in 25 cities with trained volunteers and professional supporters. Their service is linked to Oncoguida in collaboration with the Italian Ministry of Health where patients are helped to evaluate a best location for diagnosis, treatment, psychological support, rehabilitation, and care and pain control. The website (115) lists the number of cancer operations performed in each centre by the type of cancer and states explicitly that the higher the number of operations then the greater the quality of outcomes associated with that centre (116). The Oncoguida website allows individuals to enter their disease type, their location and evaluate the performance of their chosen institution.
In the UK, the Royal College of Surgeons and a large number of associated specialist surgical societies have worked together with the NHS to record and publish data on the outcomes of surgical procedures, including cancer surgery (117, 118). An example of a report that can be accessed by a patient to examine the performance of a cancer service through the “My NHS” website (119) is shown in Tables 4-7.
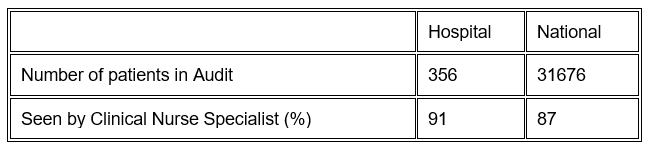
It may be helpful to consider the questions a patient may wish to ask of the information system to complement their discussions with their cancer care team. Our examples refer to a patient recently diagnosed with colorectal cancer (CRC). A patient may be interested in the level of support that is available to them in addition to the medical and surgical consultations. A good indicator of this is the availability and access to a Clinical Nurse Specialist (CNS). The data in Table 4 from MyNHS gives the percentage of patients who are seen by a Clinical Nurse Specialist in this hospital and compares that figure to the national figure for the same disorder. Accessing this data allows a patient to be reassured that they will have a level of access to this important resource which is comparable to, and perhaps better than, that available nationally. They will also know that the service and these professionals are readily available and that therefore they can reasonably ask to meet a CNS.
Table 4. A newly diagnosed patient with colorectal cancer who wants to see a CNS
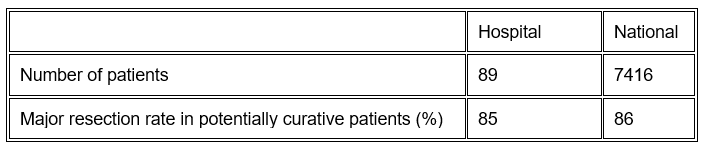
If a patient, for example, is being managed for CRC and they want to be informed about the proportion of patients who receive potentially curative major surgery, they could access the information shown in Table 5. This shows that the major resection rate in potentially curative patients for CRC in this particular hospital is high and at the national average, offering useful reassurance.
Table 5. The resection rate in a hospital for all patients deemed potentially curative
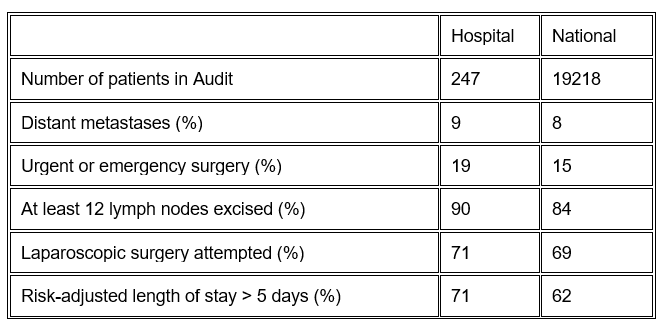
If a CRC patient is concerned about the technical performance of the surgeons in the hospital which will provide their care, then the information in Table 6 could be accessed which highlights important indicators of the technical approach performed in the hospital. For example, the number of lymph nodes excised is a recognised indicator of the completeness of surgical resection and this is seen to be relatively high in this particular hospital Trust. The use of laparoscopic surgery is an important way of minimising patient discomfort and should be used when appropriate and it is seen to be used in a relatively high proportion of patients in this hospital, at or slightly above the national average.
Table 6. Information for CRC patients having a major resection
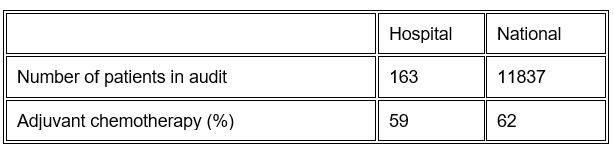
The use of adjuvant chemotherapy following major resection for stage 3 colon cancer is an important part of multidisciplinary care and significantly increases cure rates. Its uptake has, however, been variable across Europe. Our hypothetical CRC patient can access the data in Table 7 and will see that for their hospital, the uptake of adjuvant chemotherapy is slightly lower than the national average, which might prompt them to look at alternative institutions or perhaps more readily to check carefully with their multidisciplinary team in each consultation that they will be considered appropriately for adjuvant chemotherapy using standard national and international guidelines.
Table 7.The proportion of CRC patients having major resection for stage III colon cancer who then receive adjuvant chemotherapy